For many expecting parents, an approaching due date is time to feather the nest. We complete our registry, set up a nursery, and make sure we have all the baby gear we are going to need. When my first daughter was born, I was caught off guard – floored – by two surprises. One, I knew I would love her, but I didn’t know I would be IN LOVE with her. Second, the postpartum stage was harder than I expected. Much harder. I had dreamy moments of nursing in the glider and cuddling her in a carrier. But there were a lot of challenges I never even dreamed of. Breastfeeding was much harder than I expected, yet I felt strongly, almost rigidly, that it had to be 100% of her nourishment. Having things not go as expected is one of the most common risk factors for postpartum mental illness. And as we know, birth and babies rarely stick to the textbook. The “baby blues” hit 85% to 90% of new mothers, typically on day 4 postpartum, when hormones take a massive drop. This stage usually lasts about two weeks, and is considered “normal.” Even though it is “normal,” we can still make it better! In my private practice, I love to work with expecting parents during pregnancy to prepare for this postpartum stage, so that you can focus on the light and love. I’ll talk more about how you can prepare, but first: If you are having thoughts of hurting yourself, your baby, or anyone else, DON’T WAIT – GET HELP NOW. Call your OB, your mental health provider, a local hotline, or the National Suicide Prevention Lifeline (1-800-273-8255.) If you are struggling with other strong and disturbing thoughts, such as resenting the baby or regretting having a child, don’t wait. If you find that “the blues” are hanging around past two weeks postpartum, reach out and get help. You may want to be screened for a postpartum mental illness, such as postpartum depression, anxiety, OCD, or psychosis. The Postpartum Support International Warmline provides non-emergency support in English and Spanish at 1-800-944-4773(4PPD).
Making a Postpartum Plan for Mental Wellness
The first thing to understand is that Western culture does everything WRONG to support new moms. In what I call the “reverse Cinderella” effect, a pregnant woman goes from weekly OB visits to “we’ll see in you six weeks” once the baby is out. Pregnant women are often showered with attention and help, while a new mom takes back stage to the new born. Neither does our culture support new families. Nuclear families are isolated away from the family, friends and communities that could support them. Look at any traditional culture, and there are systems in place to nurture the new mom and the new dad. The community steps in to take over the duties of both parents, so they can focus on the newborn and bond. Don’t get me started on the lack of paid family leave in the US… but do think about how you can pull your community around you. It truly takes a village to support a new family. Do you ever think that you “should be strong” or “shouldn’t have to ask for help”? Let it go. PLEASE ask for help. Have a friend organize a meal train. Let someone clean your house. Register for a postpartum doula instead of toys. Ask for help and be very specific. Many friends will say, “Let me know if there is anything I can do…” Take them up on it. For more specific, practical things you can do to build your village and better survive the postpartum stage, see this short video here. My friend Andrea Knox, LMFT, sits on the board of San Diego’s Postpartum Health Alliance with me, and recently shared her 8 S’s to consider for a postpartum plan. Read it here. For an article on 7 ways to find your circle of support when pregnant or postpartum, click here.
When Is Professional Help Needed?
So far, much of the above advice is for straightforward things we can do on our own. But when do we need to reach out to a mental health professional? Apart from serious thoughts of suicide or harming another person, which need immediate help, some mothers are unsure of what is “normal” baby blues and what is too much. I like to say that whatever is too much for you is too much. If you are interested in a checklist of possible signs or symptoms of Postpartum Depression, try this page from the Postpartum Stress Center. In general, the majority of “baby blues” naturally resolve after two weeks. If signs and symptoms of anxiety or depression persist after two weeks, reach out to your doctor, the Postpartum Support International Warmline (1-800-944-4773), or a mental health professional. My practice is in San Diego, where the Postpartum Health Alliance sponsors a warmline and directory of therapists who specialize in perinatal mental health. Consult this list of Postpartum Depression treatment programs and specialists on Postpartum Progress to find a provider elsewhere in the US, Canada, UK, Australia and Switzerland. There is no harm in reaching out if you aren’t that severe. Getting support sooner is always better! _________________________
Please use caution when attempting any of the carries, exercise or activities highlighted on this blog, social media or any other content channels. Please use common sense and caution when using a baby carrier. You should consult a physician before starting any diet or exercise program. For more information, see our disclaimer.
Summer adventures with your baby are a wonderful way to create lasting memories and enjoy the beauty of nature together. From baby carriers to strollers, Ergobaby products are designed to provide comfort and ease for both you and your little one. So, gear up, get outside, and explore the world with your baby by your side.
Ready to embark on your own summer adventures? Check out Ergobaby’s range of baby carriers and strollers to find the perfect match for your family’s needs. Visit our website today and start planning your next outdoor excursion!
Emotional Benefits of Getting Outside
Spending time in nature with your baby can strengthen the bond between you. The simple act of holding your baby close, feeling their warmth, and sharing new experiences together can create strong emotional connections. It’s also a wonderful way to reduce stress and improve your mood. When my littles were extra fussy, I’d take a walk around the neighborhood. Even though I don't live in an area with trails and surrounded by nature, simply behind outside changed everything. A little vitamin D does wonders!
Cognitive Development
Nature is a sensory wonderland for babies. The different sights, sounds, and smells can stimulate your baby’s senses and promote cognitive development. Watching leaves rustle, hearing birds chirp, and feeling the texture of a tree bark can all contribute to their learning and development.
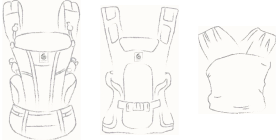
All About Baby Carriers for Nature Adventures
Choosing the Right Baby Carrier
When it comes to selecting the best baby carrier for summer adventures, there are several options to consider.
Types of Baby Carriers:
- Wraps: Perfect for newborns, providing a snug and secure fit.
- Slings: Ideal for quick and easy use, offering good ventilation.
- Soft Structured Carriers: Versatile and comfortable for both parent and baby, suitable for longer trips.
Factors to Consider:
- Baby’s Age and Weight: Ensure the carrier is appropriate for your baby’s size and weight. For example, Ergobaby’s Embrace Newborn Carrier is perfect for the fourth trimester where baby is small and you’re looking for an easy way to stay close. As they grow, you’ll want to upgrade to an all-position carrier that’s meant for growing babies.
- Parent’s Comfort and Ergonomics: Look for carriers with padded shoulder straps and lumbar support if you’re planning on longer outings.
- Ease of Use: Choose a carrier that is easy to put on and take off.
- Climate and Breathability: Opt for carriers made of breathable fabrics to keep you and your baby cool in hot weather.
Safety Tips:
- Proper Positioning: Ensure your baby is seated correctly, with their legs in an "M" position and their head should be close enough to kiss.
- Checking for Wear and Tear: Regularly inspect your carrier for any signs of damage.
- Ensuring Adequate Support: Make sure the carrier provides proper support for your baby’s head and neck.
Exploring Nature with a Baby Carrier
Ideal Spots for a Nature Walk with Baby
- Parks and Gardens: Great for leisurely walks and picnics.
- Nature Trails and Forests: Perfect for more adventurous outings.
- Beaches and Lakesides: Wonderful for enjoying the water and sand, with the right carrier.
Activity Ideas
- Hiking: Enjoy a scenic hike with a hiking baby carrier that offers support and storage.
- Bird Watching: Use your carrier to keep your baby close while you explore and observe wildlife.
- Picnics: A carrier can free up your hands, making it easier to carry picnic supplies.


Advantages of Using Strollers for Nature Adventures


While baby carriers are fantastic for mobility and closeness, depending on the adventure of choice you might want to be a stroller along too.
There are a LOT of baby stroller options on the market. So we understand how confusing it can be to choose the one that’s right for your family. Not only are there a variety of brands, but a variety of strollers that serve different purposes.
There are a few types of strollers on the market:
- Full-sized stroller: This is typically the stroller parents thing of buying for all its versatility.
- Lightweight or umbrella stroller:These compact strollers are perfect for on-the-go adventures.
- Jogging stroller: Designed for parents who want to combine fitness with outdoor adventures.
- Double stroller: Designed for parents with multiple kids, especially twins.
- Car seat carrier: These strollers connect to a specific car seat. We don't typically recommend these as they can be unsafe for baby and uncomfortable for parents who are pushing.
Learn more about the types of strollers and which one would be best for you.
Benefits of Bringing a Stroller
- Storage Space for Gear: Ample room for carrying all your essentials like a diaper bag, beach toys and more.
- Shade and Weather Protection: Built-in canopies to shield your baby from the sun when they are lounging.
- Options: If you have more than one kid, you can stroll with one and carry the other. Or, if you’re getting warm or your little one is getting fussy, you can switch up their position from stroller to carrier or vice versa.
Safety Tips for Strollers
- Ensure your stroller is in good working condition. Make sure buckles are still buckling and that there are no rips or holes that could compromise your baby’s safety.
- Use sunshades or bug nets to protect your little one’s skin.
- Securing the baby properly: always buckle up your baby for safety even if you think they are old enough to go without the buckle.
Combining Baby Carriers and Strollers
For the ultimate flexibility, consider using both a baby carrier and a stroller on your outings.
Combining both options allows you to adapt to different situations. Use the carrier for more rugged trails and switch to the stroller for smoother paths or when your baby needs a nap.
Transition Tips
- Smooth Transitions: Plan stops where you can easily switch from carrier to stroller.
- Pack Light: Only bring essentials to make transitions easier.
Tips for a Successful Adventure
Planning Ahead
- Route Planning: Choose baby-friendly trails and parks. Check local mom groups or outdoor groups and get recommendations for the best outings for kids.
- Check Weather Conditions: Avoid extreme heat or unpredictable weather. Even with our most breathable carriers, when it’s hot, it’s hot. And having two bodies against each other in the heat will be naturally hot and sticky already.
- Packing Checklist: Include diapers, snacks, water, sunscreen, and a first-aid kit. These all-position carriers have storage pockets where you can fit some of the items easily!
- Stay Hydrated and Nourished: Pack healthy snacks to keep energy levels up and bring plenty of water for both you and baby.


Summer adventures with your baby are a wonderful way to create lasting memories and enjoy the beauty of nature together. From baby carriers to strollers, Ergobaby products are designed to provide comfort and ease for both you and your little one. So, gear up, get outside, and explore the world with your baby by your side.
Ready to embark on your own summer adventures? Check out Ergobaby’s range of baby carriers and strollers to find the perfect match for your family’s needs. Visit our website today and start planning your next outdoor excursion!