Jump to a Section:
Baby Blues or PPD?
Almost every caregiver will experience the Baby Blues at some point. You’re joyful one moment, crying the next, overwhelmed, and exhausted. That’s all very normal. But if these feelings persist and last for weeks on end, it’s now considered PPD.What is Postpartum Depression?
This depressive illness affects around 15% of mothers and around 10% of fathers. That’s just based on parents who are formally diagnosed. Why are these mental health disorders on the rise? I love what Dr. Rosie Knowles of Carrying Matters has to say:Parents are encouraged to put their babies down as much as possible and regain their old lives; babies are expected to learn independence as quickly as possible and stop relying on their parents for their every need. This approach to caring for children is very new in human history and runs counter to attachment theory, which suggests that the human infant thrives on responsive parenting and close contact…. …Western society is increasingly fractured and isolated, with a decreased sense of local community and shared care. Depression is common in our culture, for reasons not clearly understood, but partly due to the way we live. The birth of a baby is often an overwhelming time for both parents, especially when also faced with the expectations and demands of a fast-paced culture that often judges people by their apparent productivity and appearance.
Primary Symptoms of Postpartum Depression
- Mood swings
- General Anxiety / Panic attacks
- Severe lack of energy or motivation (months after birth)
- Constant crying
- Forgetting to eat / overeating
- Inability to sleep, especially due to worry over baby
- Overly fearful of being a "bad" parent
- Obsessive Handwashing
- Declining opportunities to leave the house
- History of mental health challenges
- Challenges with pregnancy, labor and delivery
- Recent stressful life events
- Lack of support
What to Do if You Suspect You Have PPD
1. Tell Someone Telling someone is the first step in getting help and is often the most difficult. Letting your partner, a family member, or a close friend in on what you’re going through opens the door for them to offer help. Whether it’s watching your little one so you can nap, helping with laundry, cooking a meal, or helping you get outside, these little things add up and make a huge difference. Shop Sleep Products 2. Contact Your Care Provider Your medical practitioners, doula, or other care providers can recommend next steps for you. Prescription medication may be a necessary solution and is 100% ok! Taking care of yourself is a priority. 3. Get Outside and Get Moving
When we’re in bouts of depression, nothing sounds better than laying in bed for days on end. And while it’s ok to feel that way, it’s important to push through and let the sun shine on your face. Get your body moving as much as possible, that’s safe for your body post-delivery. Everyone is different. Don’t push too hard. Give yourself grace.
There also exists a range of less scientifically investigated stress management tools, which include elicitation of the relaxation response, breath focus, guided imagery, touch therapy, bright light therapy, acupuncture, mindfulness meditation, yoga, tai chi, qigong, healthy eating, repetitive prayer, social support and diary-keeping.
SHOP METRO+ STROLLER
4. Keep Talking
If you’ve told even just one person about your mental health, keep talking to them. Check in. Share if you’re having a good day or a low day. Ask them to help. And keep asking. It’s never too much.
5. Get A Baby Carrier
In recent studies, mothers providing daily skin-to-skin contact to their newborn had significantly lower scores on the depression scales (indicating that they were less depressed) when the infants were one week and marginally significantly lower scores when the infants were one month, but no significant differences at 2 and 3 months, where depressive symptoms were few for both groups. The depressive symptom scores were below the risk zones for most of the mothers in both groups. Some mothers, however, scored in the risk zone for depression, and were hence suffering the most. These mothers were virtually all in the control group, who did not engage much in skin-to-skin contact.
Read more about how babywearing can help alleviate postpartum depression.
3. Get Outside and Get Moving
When we’re in bouts of depression, nothing sounds better than laying in bed for days on end. And while it’s ok to feel that way, it’s important to push through and let the sun shine on your face. Get your body moving as much as possible, that’s safe for your body post-delivery. Everyone is different. Don’t push too hard. Give yourself grace.
There also exists a range of less scientifically investigated stress management tools, which include elicitation of the relaxation response, breath focus, guided imagery, touch therapy, bright light therapy, acupuncture, mindfulness meditation, yoga, tai chi, qigong, healthy eating, repetitive prayer, social support and diary-keeping.
SHOP METRO+ STROLLER
4. Keep Talking
If you’ve told even just one person about your mental health, keep talking to them. Check in. Share if you’re having a good day or a low day. Ask them to help. And keep asking. It’s never too much.
5. Get A Baby Carrier
In recent studies, mothers providing daily skin-to-skin contact to their newborn had significantly lower scores on the depression scales (indicating that they were less depressed) when the infants were one week and marginally significantly lower scores when the infants were one month, but no significant differences at 2 and 3 months, where depressive symptoms were few for both groups. The depressive symptom scores were below the risk zones for most of the mothers in both groups. Some mothers, however, scored in the risk zone for depression, and were hence suffering the most. These mothers were virtually all in the control group, who did not engage much in skin-to-skin contact.
Read more about how babywearing can help alleviate postpartum depression.
The Perfect Baby Carrier For You
When it comes to simplifying life with a newborn, babywearing is a must. Not only does it help you and your little one bond, it gives you the ability to be hands free and mobile! Go for walks, meet up with a friend, or even let a family member or friend carry the baby for a little bit so you can nap! Our baby carriers are designed to support you wherever you're at in your parenting journey. Embrace Available in two fabric ways, Ponte Knit and Soft Air Mesh, Embrace is designed to support you in your fourth trimester journey. Safe for newborns through 25 lbs, it's the perfect way to stay cozy and comfortable from the start.
SHOP EMBRACE CARRIERS
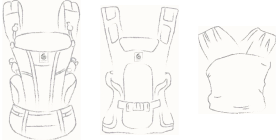
Omni
Our Omni carriers feature all four carry positions (inward, outward, back, hip) and can be used from 7lbs through 45lbs. Available in two fabrics (Breeze for ultimate breathability and Dream for unparalleled softness), these all around baby carriers keep you and your little one close on adventures big and small.
SHOP OMNI CARRIERS
Aerloom
Made to move, stretch, and fit your daily life, this first-of-its-kind carrier redefines comfort. Ultra-lightweight with built-in airflow and constructed from FormaKnit™ fabric (made from post-consumer materials) creates the ultimate fit. Safe for newborn through 3 years.
SHOP AERLOOM CARRIERS
Available in two fabric ways, Ponte Knit and Soft Air Mesh, Embrace is designed to support you in your fourth trimester journey. Safe for newborns through 25 lbs, it's the perfect way to stay cozy and comfortable from the start.
SHOP EMBRACE CARRIERS
Omni
Our Omni carriers feature all four carry positions (inward, outward, back, hip) and can be used from 7lbs through 45lbs. Available in two fabrics (Breeze for ultimate breathability and Dream for unparalleled softness), these all around baby carriers keep you and your little one close on adventures big and small.
SHOP OMNI CARRIERS
Aerloom
Made to move, stretch, and fit your daily life, this first-of-its-kind carrier redefines comfort. Ultra-lightweight with built-in airflow and constructed from FormaKnit™ fabric (made from post-consumer materials) creates the ultimate fit. Safe for newborn through 3 years.
SHOP AERLOOM CARRIERS
How to Help Someone with Postpartum Depression
 1. Listen
Now isn’t the time to solve problems. It’s just time to be a safe space for this person to share what they are experiencing. Reassure them that it’s ok. You hear them. And you are here to support them however they need it. Additionally, if you had PPD or know someone who did, don’t compare experiences. Let this person’s feelings be valid on their own.
2. Make Specific Plans
Offering to help is huge, but open-ended statements like “let me know how I can help” leaves the ball in the parent’s court and chances are, they won’t speak up. OR, they don’t really know what would help. Instead, offer specific ways at specific times. “I will come over tomorrow and make dinner.” “I will come over Friday and hold your baby so you can nap.” Make plans and follow through!
3. Encourage and Support
Offer encouragement whenever you’re with this parent. Notice when they seem to be having a good day or improving. Support them when they decide to seek treatment or take a specific course of action. Continue to be a listening ear.
1. Listen
Now isn’t the time to solve problems. It’s just time to be a safe space for this person to share what they are experiencing. Reassure them that it’s ok. You hear them. And you are here to support them however they need it. Additionally, if you had PPD or know someone who did, don’t compare experiences. Let this person’s feelings be valid on their own.
2. Make Specific Plans
Offering to help is huge, but open-ended statements like “let me know how I can help” leaves the ball in the parent’s court and chances are, they won’t speak up. OR, they don’t really know what would help. Instead, offer specific ways at specific times. “I will come over tomorrow and make dinner.” “I will come over Friday and hold your baby so you can nap.” Make plans and follow through!
3. Encourage and Support
Offer encouragement whenever you’re with this parent. Notice when they seem to be having a good day or improving. Support them when they decide to seek treatment or take a specific course of action. Continue to be a listening ear.
Support Groups
https://reddit.com/r/beyondthebump/ https://www.postpartum.net/get-help/locations/ https://www.samhsa.gov/find-help/national-helpline https://www.postpartumdepression.org/support/groups/ https://psichapters.com/|
If you or someone you know is experiencing any Maternal Mental Health issues, the National Maternal Mental Health Hotline is available 24/7, 365 days a year in English or Spanish and other languages by request. Powered by Postpartum Support International, this is a first-of-its kind resource made possible with the support of the U.S. Health Resources and Services Administration. The hotline is staffed by licensed and credentialed perinatal mental health and healthcare providers, childbirth professionals, and certified peer specialists, and provides immediate and informed access to support, understanding, brief intervention, and resources to all pregnant, postpartum, and post-loss individuals AND their partners and families. Call or text the Hotline anytime to connect. You do not need a diagnosis to reach out for help. National Maternal Mental Health Hotline: 1-833-943-5746 |