
Here you are — you finally think you have this breastfeeding thing down. No more sore nipples, baby is gaining weight, sleeping in longer stretches, and you’re finally starting to feel like your old self again. Then suddenly you have a drop in your milk supply in what seems like overnight. This sudden change isn’t uncommon to nursing mothers, but it can cause momentary panic in a new mom and leave you wondering why this is happening. Many things can cause a once robust milk supply to drop. It could be that you went back to work and are now separated from your baby for longer stretches during the day, perhaps you had an illness, have had recent stress in your life, return of your menstrual cycle, or just plain haven’t been taking good care of yourself. Whatever the reason for this drop, there are things you can do to increase your milk supply and bring it back up to the level it once was.
Can you increase your milk supply after it decreases?
Yes. The fastest way to increase your milk supply is to ask your body to make more milk. Whether that means nursing more often with your baby or pumping – increased breast stimulation will let your body know you need it to start making more milk.
How long does it take to increase your milk supply?
It usually takes about 3-5 days before you see an increase in your supply.
Here are 10 tips on how to increase your milk supply and get it back up to where it once was:
1. Get lots of rest and take care of yourself. It is so important that you’re getting enough sleep. Try to choose a sleeping arrangement that allows for the maximum amount of sleep for mom and baby. Have the right swaddler or sleep sack for the age of your child. This ensures they’re not only as comfortable and warm as possible, but these kinds of products are specifically designed to help your baby feel safe and secure to help them sleep longer and better.
2. Drink lots of water! I can’t stress this enough. Every time you breastfeed or pump, drink a glass of water.
3. Have a “nurse in” with your baby. Take at least 24 hours and snuggle in with the baby. Have water, snacks and diapers at hand and nurse as often as baby will nurse. Be sure to have a comfortable nursing pillow to make the experience as comfortable as possible for you and your baby. Practicing skin to skin during this time also helps to increase milk supply. This time together for mom and baby not only will increase the frequency of nursing, but also provide some extra rest for Mom, which also helps to increase prolactin level and helps with your milk supply.
4. Consider pumping. Try to pump 8-10 times in 24 hours, 10-15 minutes at a time, every day after breastfeeding until you notice your supply increasing. You’re pumping to increase your milk supply, so don’t worry if nothing comes out at first.
5. Apply a warm compress to your breasts for a few minutes before breastfeeding or pumping. Combined with a breast massage, the warm compress will help to get the milk flowing.
6. Try taking galactagogues. Galactagogues are herbal supplements that help to get your milk supply back. The most commonly used are Fenugreek, brewers yeast, blessed thistle and alfalfa. Before taking a galactagogue talk to your health care provider to see if they are safe for you.
7. Take away the pacifier. If your baby has a need to suck – let them fulfill that suck on your breasts. Any extra stimulation on your breasts will help to increase your milk supply.
8. Eat foods know to help increase your milk supply. Foods such as oatmeal, garlic, carrots, fennel, nuts, green papaya, sesame seeds and ginger all work to help increase your milk supply.
9. Make lactation cookies. There are many recipes online that are easy to make and yummy to eat. These cookies contain ingredients that will work to give your supply a boost.
10. Don’t stress out. Try to keep things relaxed and focus on the positive things. Your milk supply will return.
Breastfeeding is incredible and beautifully beneficial. But it doesn’t come without its challenges and questions. There are a lot of common breastfeeding concerns among nursing mothers everywhere! Here are the answers to the most commonly asked breastfeeding and milk supply questions.
What is colostrum and why is it important?
Colostrum is the first milk your body produces. It’s a milky fluid that’s usually yellow/gold in color and thicker than breast milk. It usually lasts for 2-4 days after giving birth.
Some call it the baby super food because colostrum is high in protein, vitamins, minerals and antibodies, all of which help build and support your newborn’s immune system. It fights infection, supports your baby’s immune system and gut function and can help prevent jaundice.
When does your milk come in?
For most mothers, they make colostrum for the first 2-4 days after birth. Breast milk typically comes in around day 3, 4 or 5.
Is it normal to have an uneven milk supply?
Yes. It’s relatively common for one breast to produce more milk than another one. You might even notice your breasts are different sizes. There is no cause for concern as long as you’re comfortable and your baby is eating well and comfortable, too.
You can ask and look into tips about how to produce more breast milk in your breast that isn’t producing as much.
How to increase milk supply when pumping?
- Pump more often
- Pump after nursing
- Pump both breasts at once
- Make sure you have good pumping equipment and that it’s working properly, i.e. learn how to use it, keep it clean, make sure you’re using the correct size of breast shield and speed
- Have a comfortable, dedicated space to pump
- Talk to a lactation consultant
6 Top Tips for Boosting Milk Supply
What affects breast milk?
- Stress and anxiety levels
- Not eating or drinking enough
- Supplementing with formula for multiple feedings a day
- Accompanying symptoms of getting sick, i.e. dehydration, vomiting, diarrhea, fatigue
- Certain medications or herbs
- Infective latch
- Not breastfeeding enough
- Hormonal or endocrine problems, such as PCOS, thyroid problems, diabetes
What should I eat and avoid while breastfeeding?
You need extra calories when breastfeeding (the amount depends on the mom’s lifestyle). Try to get those extra calories from nutritious foods, such as fruits, vegetables, lean meats and poultry, whole grains, dairy products (if your baby isn’t dairy intolerant).
- Foods and drinks you probably want to say no to:
- Foods that can give you gas, i.e. spicy foods, cabbage, broccoli, beans, etc.
- Fish that are high in mercury and other contaminants
- Fatty foods
- Alcohol
- Sugary drinks
- Caffeinated drinks (in moderation, too much may or may not affect you and baby)
- Milk (baby may have a dairy allergy or intolerance)
Will I have a menstrual cycle while breastfeeding?
It’s common not to have a menstrual cycle while breastfeeding because of hormonal changes. Every woman’s body is different if and when you have a menstrual cycle or when yours will return while or after breastfeeding. Some women get their periods back when their baby starts eating solid foods and they’re breastfeeding less.
How to dry up breast milk supply?
There are a few different ways to dry up your supply if you’re ready to stop breastfeeding or if your little one is weaning. Some women’s milk supply dries up in only a few days. For others, it may take weeks or months to completely dry up. Here are the most common:
- Stop breastfeeding. Use ice packs to help with any inflammation and occasionally hand express some milk to relieve engorgement. Some moms say to apply cabbage to help soothe engorged breasts, too.
- Go an hour or two longer between pumping sessions.
- Using certain birth controls and herbs have been shown to stop milk production.
What are the benefits of breastfeeding?
- The CDC has a list of benefits on its website for infants and mothers.
How often and long should you breastfeed?
- On average, newborns breastfeed 8-12 times a day, about every 2-4 hours, during the first few months of life. Some may cluster feed and nurse every hour, while other babies can go 3-5 hours during their longer stretches of sleep.
- As babies get older and as they start eating solid foods, the number of times they nurse a day will decrease.
- Every baby is different. Feeding on demand is recommended for newborns, and then as your baby gets older they should have a more predictable feeding schedule.
- The American Academy of Pediatrics and the World Health Organization recommend exclusively breastfeeding for a baby’s first 6 months of life and then for up to 2 years old or longer, along with offering solid foods as appropriate.
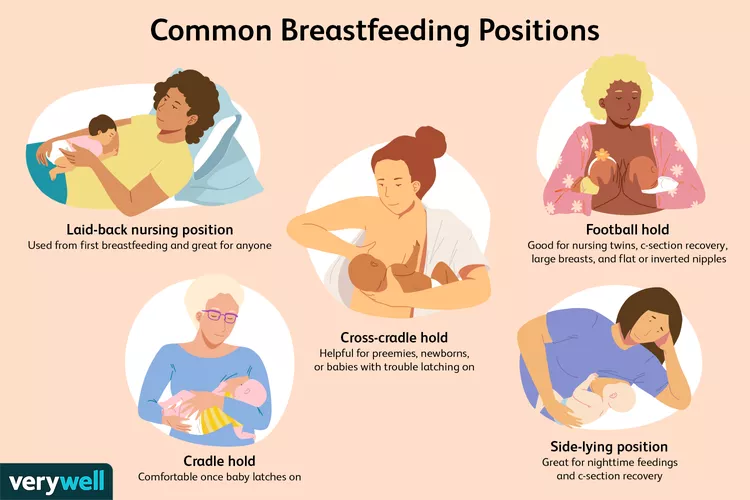
What are the (best/most common) breastfeeding positions?
- Cradle hold
- Cross-cradle hold
- Football hold
- Laid-back position
- Side-lying position
- Breastfeeding in a carrier
How do you store breast milk?
- Freshly expressed or pumped breast milk can be stored:
- For up to 4 hours at room temperature
- In the refrigerator for up to 4 days (the coldest part of the fridge is best)
- In the freezer for 6 months, in some cases up to 12 months
- Previously frozen, now thawed, breast milk can be stored:
- For 1-2 hours at room temperature
- For 1 day in the refrigerator
- Breast milk can be stored in clean storage bags, food-grade containers or bottles.
- Be sure to label the breast milk with the date it was expressed/pumped.
We hope this list of commonly asked breastfeeding and milk supply questions and answers was helpful. We also encourage you to find your own personal support system of other breastfeeding moms and a lactation consultant to help you along your breastfeeding journey.



